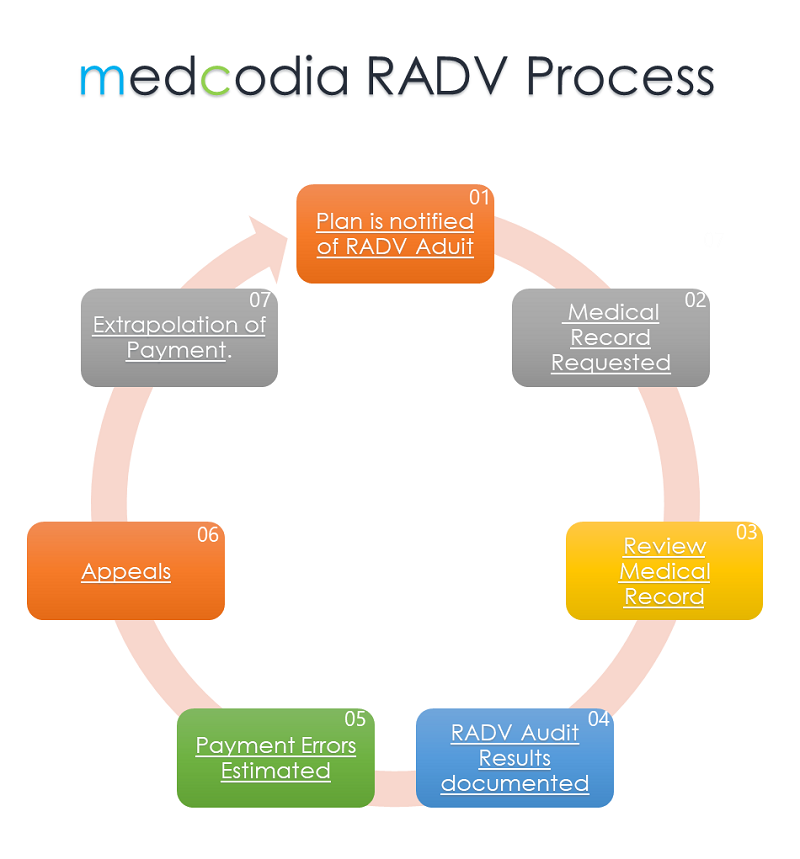
medcodia RADV Process
RADV = Risk Adjustment Data Validation Audit: CMS process that ensures the integrity and accuracy of the providers data submission to substantiate risk adjustment. The goal of the RADV Audit is to identify any discrepancies by comparing risk adjustment diagnosis data submitted by a Medicare Advantage (MA) organization via encounters and claims, against the data provided to CMS per the RADV audit process.